A 58 year old female patient
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
Cheif complains
The patient presented to the OPD with the chief complaints of Vomiting since 8 days, Decreased appetite and fever since 6 days and SOB from 3 days
HOPI
The patient was apparently asymptomatic 8 days back Then she developed vomitings and the contents are The food consumed prior.she developed decreased appetite six days back.Fever since six days which is intermittent and is relieved on medication.
PAST HISTORY
k/c/o DM type 2 and HTN since 20 years
VITALS
BP-130/80 mm of hg
PR-87/min
RR-20/min
afebrile
SYSTEMIC EXAMINATION
CVS:S1S2 heard
Jvp not raised
No murmurs heard
RESPIRATORY:grade 3 dyspnea
ABDOMEN: Normal
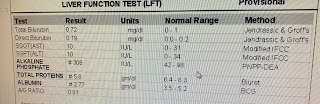
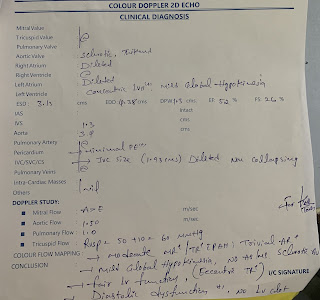
INVESTIGATIONS
PROVISIONAL DIAGNOSIS
uncontrolled type 2 DM
TREATMENT
-normal soft diabetic diet
-IVF -NS/RL 75 ml
-INJ. HAI acc to GRBS
-INJ OPTINURON 1 amp
-INJ ZOFER 4mg IV/OD
-INJ LASIX 20 mg IV/BD
T.MET XL 25 mg PO/OD
Strict GRBS monitoring second hourly












Comments
Post a Comment