This is an online Blog book to discuss our patients deidentified health data shared after taking his/ her guardians to sign an informed consent
Here we discuss our patient problems through a series of inputs from the available Global online community of experts with n aim to solve those patient clinical problems with the current best evidence-based input
This Blog also reflects my patient-centred online learning portfolio.
Your valuable input on the comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competence in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
CASE:-
A 65 year old male, tractor driver by occupation, came to the OPD with complaints of vomitings, diarrhoea and fever since 5 days.
HISTORY OF PRESENT ILLNESS:-
The patient started developing these symptoms 5 days ago. He was at home when he got up from his bed and started vomiting (projectile) with the vomit comprising food or water, depending on what he consumed. He came to the hospital on the same day (6.10.2022) with complaints of projectile vomiting. He had 4-5 such episodes in one day. Even after vomiting everything that he consumed (in an episode), he still retched afterwards 3-4 times with no vomit. He then passed watery, greenish stools 4 times that day which was associated with squeezing type of pain in the epigastric region and developed a high grade fever. He also had associated shortness of breath. He came to this hospital on the same day, was medicated for it and discharged the next day.
The symptoms, however, did not subside and the patient was rushed to the ICU at 4pm on 9.10.2022 with complaints of vomiting and not being able to consume anything without vomiting. He hasn't been passing any stools till 9:30am yesterday.
PAST HISTORY:-
He has been having joint pains since 10 years and has been going to the hospital repeatedly for his pains. He took painkillers and continued to work everyday till 4 days ago.
He is a known case of diabetes mellitus and hypertension since 8 years, for which he has been taking medicines regularly.
5 years ago, he had a sudden rise in his blood sugar levels, causing him to become faint. He was admitted in LB nagar and then transferred to our hospital for further treatment.
From 3 years ago, the patient has been getting scaly, itchy rashes with peeling of skin on his arms and legs. He was told this was due to diabetes.
2 years ago, he fell while riding a bicycle. He fell with his left arm extended and landed with impact on his palm. He later developed a swelling on the dorsum of his hand, the contents of which were removed with a needle at a local hospital. The swelling however recurred and grew in size. The patient was told that surgery was the only option to remove the swelling but not preferred in this patient due to diabetes.
He also had asthma since 6 months for which he uses an inhaler whenever he gets an attack.
TREATMENT HISTORY:-
PERSONAL HISTORY:-
Diet: mixed
Appetite: decreased
Sleep: decreased
Bowel movements: decreased
Micturition: decreased
Addictions: patient regularly chewed betel leaf since 15 years
GENERAL EXAMINATION:-
The patient is obese and well nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema present
Vitals:-
Temperature: 98.6°F
Blood pressure: 100/60 at time of admission
Pulse rate: 84bpm
Respiratory rate: 20/min
Spo2: 98%
GRBS: 121mg%
The swelling on the dorsum of his left hand is 4×5 cm in size, elliptical, firm, non-reducible. Slip test is positive.
SYSTEMIC EXAMINATION:-
CVS: S1 S2 sounds heard
No palpitations or murmurs.
Respiratory system: position of trachea is central, vesicular breath sounds heard.
Abdomen: abdomen is distended and umbilicus is central, everted. Tenderness in the right hypochondrial and epigastric regions. Liver is palpable.
CNS: Patient is conscious, coherent and cooperative
Glasgow coma scale: 15/15 f4v5m6
INVESTIGATIONS:-
PROVISIONAL DIAGNOSIS:-
Acute gastroenteritis
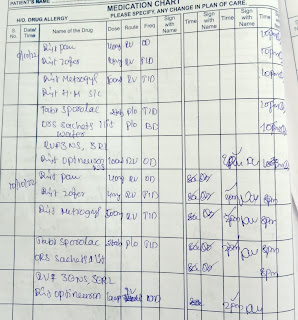
TREATMENT:-


















Comments
Post a Comment