65 year old male, farmer by occupation resident of nalgonda, stopped working 6 months ago, in view of generalized weakness,presented to the opd with chief complaints of fever since 5 days(low grade, intermittant and associated with chills). C/O weakness of right upperlimb and left lower limv since 4 days. B/L knee pain. C/O Abdominal distension and facial puffiness ,B/L pedal edema since 4 days.
No sob, chest pain, palpitations, orthopnea.
C/O giddiness and loss of appetite.
H/O loose stools 3 days ago(10-12 episodes /day for 2 days, black coloured stools) whhich subsided now associated with pain abdomen in umbilicus.
No vomitings, headache, cough. No decreased urine output.C/O burning micturition. No h/o trauma,seizures.
PAST HISTORY :
NO H/O DM, HTN, TB, Asthma, CVA, CAD.
NO H/O previous renal issues.
H/o covid pneumonia 8 months ago, subsided with in 2 days.
H/o fall 2 years back on right hand, implant placed.
H/o typhoid and liver issues which subsided with medication.
PERSONAL HISTORY :
appetite :lost
Bowel and bladder regular
Sleep decreased
Addictions:chronic alcoholic 90ml/day
Chronic chutta smoker.
GENERAL EXAMINATION :
patient is c/c/c.
Temp:Afebrile
Bp:70/50 mm Hg
PR:60 bpm
Rr:18 cpm
Spo2:98%at RA
GRBS:104 mg/dl
No pallor, icterus, clubbing,lymphadenopathy,cyanosis.
Edema present.
SYSTEMIC EXAMINATION :
CVS:S1,S2 heard, no murmurs
RS :BAE +,NVBS heard.
P/A:Distended.
No tenderness, palpable masses,bowel sounds heard.
CNS:
Power Rt. Lt
UL. 3/5. 5/5
LL. 4/5. 3/5
PROVISIONAL DIAGNOSIS :
?AKI on CKD secondary to Acute GE
Fever with thrombocytopenia with bleeding manifestations.
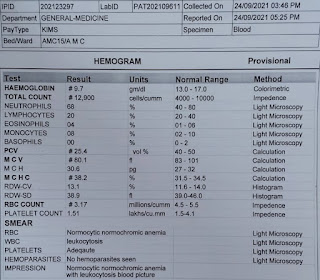
INVESTIGATIONS:
HB:11g/dl
TLC: 10,700
PLT: 81000
ESR :7mm/hr
S. CREAT:8.8
URIC ACID:7.8
TB:1.3
Na :135
K :2.6
Cl :98
Ns1 antigen :negative
PROGRESSIVELY DECREASING THROMBOCYTOPENIA
PLAN OF CARE:
IVF:NS,RL @ 50 ml/ hr
Inj. Pan 40mg iv/OD
Inj. Piptaz 4.5g/iv/stat--->2.25g iv/qid
Inj. Lasix 40mg iv/bd
Tab. Pcm 650 mg po/sos
Tab. Doxy 100mg po/bd
Tab. Nodosis 500mg po / tid
Tab. Shelcal 500mg po/OD
INJ. Optineuron 1 amp. in 100 ml NS IV /OD









Comments
Post a Comment