45 year male with dysphagia
45 year male with dysphagia
This is an online Blog book to discuss our patients deidentified health data shared after taking his/ her guardians to sign an informed consent
Here we discuss our patient problems through a series of inputs from the available Global online community of experts with n aim to solve those patient clinical problems with the current best evidence-based input
This Blog also reflects my patient-centred online learning portfolio.
Your valuable input on the comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competence in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
CONSENT AND DEIDENTIFICATION :
The patient and the attendees have been adequately informed about this documentation and the privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
A 45 year male clinically presented to the casuality with complaints of
Dysphagia since a month.
Vomiting since 15 days.
HOPI:
A 45 year male clinically presented to the casuality with complaints of dysphagia to solids, intermittent associated with retrosternal burning pain since a month. History of 1 episode of vomiting daily for 15 days, non bilious, non projectile. History of decreased intake of food since 15 days. Now admitted for further evaluation and management.
PAST ILLNESS:
Patient was apparently asymptomatic 3 years ago, then he had an alleged history of fall in well, resulting in an injury to left ankle, ultimately resulting in formation of a non healing ulcer, for which he sought for consultation and was diagnosed with Diabetes Mellitus and started on oral hypoglycemic agents.
3 months ago, he had history of typhoid and dengue fever and took treatment for the same at local hospital and relieved.
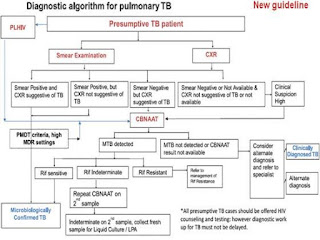
Since 2 months, the patient had complaints of productive cough, associated with scanty yellowish coloured sputum, associated with chest pain while coughing, the patient sought for consultation and was diagnosed with Pulmonary Tuberculosis based on chest x ray findings and started on ATT a month ago. The cough was relieved 15 days ago upon having medications. The patient used single drug regimen for a week from private hospital. He stopped ATT medications and went to government hospital and started on weight based ATT, but the patient was never used them.
History of low grade fever not associated with chills and rigors 10 days ago, which was relieved on taking medication.
PERSONAL HISTORY:
Appetite normal.
Sleep adequate.
Bowel and bladder are regular.
No allergies.
Chronic alcoholic: 180 ml of whisky twice weekly from the age of 22. Stopped 4 months ago.
Non smoker.
Tobacco chewing occasional.
FAMILY HISTORY:
No history of similiar complaints in family.
No Comorbidities.
GENERAL PHYSICAL EXAMINATION:
Moderately built and poorly nourished.
Patient was conscious and cooperative.
Oriented to time, place and person.
Pallor, clubbing and lymphadenopathy present.
Cyanosis, pedal edema are absent.
PR : bpm; BP: mmHg; RR: cpm; SpO2: %@RA; GRBS: mg/dl.
CVS: S1,S2+; R/S: BAE+; P/A: Soft, Non tender, BS+; CNS: NFND.
COURSE IN THE HOSPITAL:
A 45 year male clinically presented to the casuality with above mentioned complaints. Upon admission his initial GRBS was 530 mg/dl. Urine for ketone bodies and ABG was done. Mean while he was started on Intravenous Insulin therapy according to his body weight. Urine for ketone bodies was negative and ABG showed Mixed metabolic acidosis. His serum K+ was 3.0 for which 20 meq of KCL correction was given with 500ml 0.9% NS Over 4 hours. Repeat serum K+ was 3.2.
ECG AT PRESENTATION:
ABG:
CHEST X RAY PA VIEW:
INVESTIGATIONS CHART:
USG ABDOMEN:
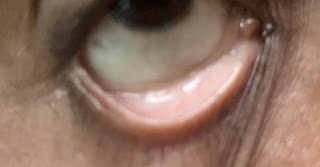
CLINICAL IMAGES:
PROVISIONAL DIAGNOSIS:
UNCONTROLLED TYPE II DIABETES MELLITUS;
PULMONARY TUBERCULOSIS.
Acknowledgment










Comments
Post a Comment